Precision Rehabilitation May Prevent Osteoarthritis
Media Inquiries
Athletes and sports fans know that a torn ACL knocks a player out of the game, requires surgical repair and involves a long recovery. But for many injured athletes, being temporarily sidelined is only the beginning of a lifelong struggle.
According to Eni Halilaj(opens in new window), an assistant professor in mechanical engineering at Carnegie Mellon University and biomechanist who specializes in orthopaedic rehabilitation, 60% of those who suffer this common knee injury also develop osteoarthritis early in life. The degenerative joint disease, which affects an estimated 32.5 million individuals in the U.S., is especially problematic for younger patients because of the longer time span during which the chronic condition can cause debilitating pain, stiffness and limited mobility.
"How can we make the 60% have the same long-term outcome as the 40%?" asked Halilaj, who is working to understand the difference between those who do and those who do not develop osteoarthritis following knee trauma.
Halilaj and her interdisciplinary team of mechanical engineers, bioengineers and computer scientists are working to integrate insights from their experimental and computational work to develop effective rehabilitation strategies aimed at restoring and preserving pain-free mobility throughout the lifespan.
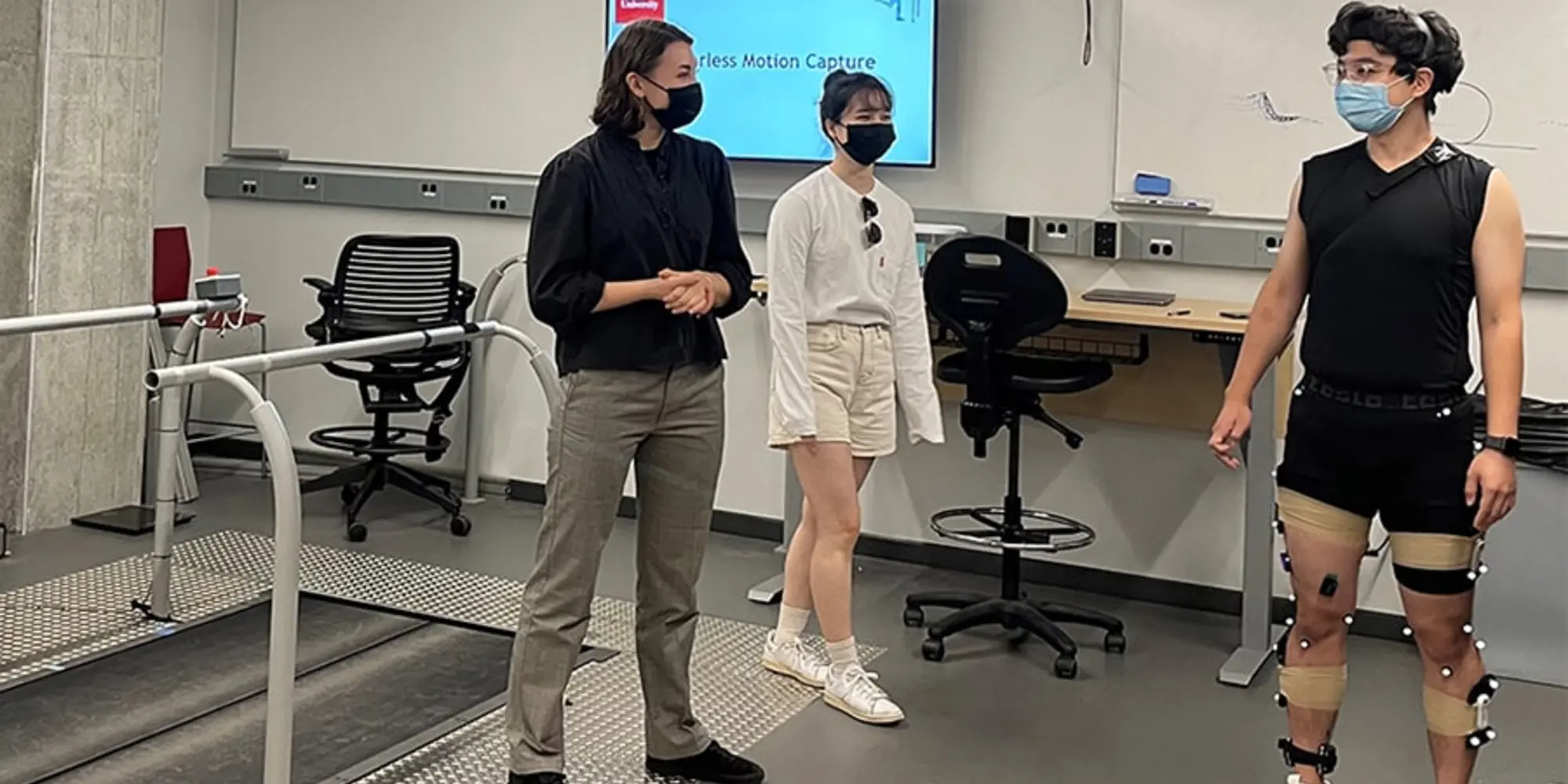
Experiments in Halilaj's motion capture laboratory focus on identifying mechanical risk factors for debilitating diseases like osteoarthritis. The 1,000-square-foot lab is outfitted with 20 cameras positioned along the ceiling throughout the room, which are used to visualize highly reflective spherical markers that are strategically placed on a human subject's body to track their motion and analyze their gait. A split-belt treadmill further analyzes the subject's motion by measuring the force exerted by each step. Electromyography (EMG) sensors are used to evaluate muscle activations during movement by measuring electrical activity produced by skeletal muscles.
While data gathered in this type of research lab is critical to identifying mechanical risk factors, patient access to such facilities is limited. Recent studies have shown that the presence of researchers observing gait analysis tests has a measurable effect on how the patients walk that could undermine the reliability of findings from traditional gait analysis studies.
The key to better insights may lie in monitoring how patients move in natural environments as opposed to specialized laboratories like Halilaj's Musculoskeletal Biomechanics Lab(opens in new window).
"Using flexible wearable sensors that look like Band-Aids, we monitor movement outside of the lab, where patients are not on their best behavior and may be adopting pain avoidance walking strategies that damage their joints in the long run," said Halilaj.
Her group is pairing wearable sensing data with advanced magnetic resonance imaging of the knee to discover the problematic walking strategies that are associated with early osteoarthritis — what she calls "digital biomarkers of osteoarthritis."
In addition to gait adaptation following surgery, physical therapy plays an important role in recovery. Recent advances in computer vision now offer untapped potential for movement analysis from video, enabling real-time tracking and feedback to improve physical therapy. Halilaj and her team are also developing open-source software that fuses computer vision algorithms with biomechanical modeling to allow accurate motion tracking from inexpensive cameras, like those embedded in personal smartphones.
Observational studies that monitor patients in physical therapy and natural environments will help researchers like Halilaj discover digital biomarkers of future disease, which can be targeted with preventative technologies in the future. Together with experts in haptics, Halilaj's team is developing wearable haptic systems to help train patients to change the way they move.
"In a not-too-distant future, we envision clinicians using data from these minimal wearables sensors and smartphone videos to isolate the 60% of patients who are likely to suffer from debilitating osteoarthritis, personalize their therapy accordingly, and even prescribe a wearable haptic device that helps them correct their gait before it is too late," concluded Halilaj.
— Related Content —
Machine Learning Algorithm Revolutionizes How Scientists Study Behavior